Kidney Transplantation
Dr Priyadarshi Ranjan, spells out some facts pertaining to kidney transplants.
Who needs kidney transplantation ?
Any patient who has established renal failure or End Stage Renal Disease (ESRD) over three months and requires dialysis needs a kidney transplant. Patients with ESRD usually have three options — kidney transplantation, haemodialysis, and Continuous Ambulatory Peritoneal Dialysis (CAPD). In some situations when doctors feel that transplant is needed in near future before beginning dialysis, patient can go for preemptive kidney transplantation
Which is better — kidney transplantation or lifelong dialysis ?
The best option is kidney transplantation, provided the family has a donor and can bear the expenses of the surgery and medicines used in the transplant. Dialysis is just a temporary bridging measure till a suitable kidney donor is found. Transplant is the only modality that can cure renal failure and help a person lead a near normal life.
What defines a successful kidney transplantation ?
Usually, if the recipient receives the kidney from a genetically related healthy individual such as a real brother, sister, parents or children, then the chance of success of a fully matched donor and recipient are around 95 per cent at the end of one year, provided there are no other adverse factors. Success also depends on how healthy is the received kidney, what is the primary disease causing the native kidney failure, how close is the match between donor and recipient and many other variables.

How long does a patient require hospital stay ?
If everything is normal and there is no adverse event then after transplant the hospital stay should not be more than 15 days for the recipient and five days for the donor.
What is the procedure for procuring kidney from a donor ?
Donor's surgery can be done in two ways. First is through a laparoscopic donor nephrectomy, with minimal incision and discomfort post surgery (donor is discharged on day three or four). The other option is open surgical donor nephrectomy in which the donor has a long incision on the flank, which is more painful and uncomfortable than the laparoscopic donor nephrectomy. Donor is discharged around the fifth or sixth day post surgery and can resume work in 15-20 days.
What are the risks involved in transplant surgery ?
Overall, more than 80-90 per cent of patients do well. Sometimes the transplanted kidney is not taken up well by the human body of the recipient, leading to rejection. Mostly, it is managed aptly with anti rejection medicines, but five to 10 per cent patients still may have major problems, such as serious life threatening infections due to lowered immunity. Some patientsmay have bleeding or other surgical complications that comprise one to two per cent risk of dying as they could lose the graft kidney, but these situations are very rare. Patients can discuss with their doctors the kind of immunosupression they require. It can always be tailored up to a certain limit according to their finances. Usually, monthly expenses are estimated at `10,000. High potency drugs to minimise rejection are takenmostly in the initial two to three years; if the initial period goes well then the intensity of immunosupression is gradually tapered, decreasing its cost. Later on even cheaper alternative drugs are available.
What is the post surgical treatment regime ?
Most of the transplant medicines are likely to get reduced or stopped after transplantation. If the patient has very severe hypertension before the transplantation and is on multiple drugs for control of blood pressure then it is likely that once the transplanted kidney starts working well, these medicines would be reduced. The patient would now require only a single antihypertensive drug or no medicines at all. Since the new kidney is capable of producing erythropoietin hormone and can balance calcium, there is no need to take injections, iron or calcium.


What are the disadvantages of lifelong dialysis ?
Long-term dialysis can lead to access related complications (infection, thrombosis, pseudoaneurysm etc), metabolic disturbances in electrolytes (predominantly sodium and potassium), transmission of blood borne infections (Hepatitis B, and C), and systemic effects (dialysis related dementia, aluminium intoxication etc).
Will the donor have any problem in his/her future life ?
After donor nephrectomy, most donors do well, except that they have to be very vigilant for the rest of their lives. Donors should be briefed that if they have any urological problems they should immediately see a doctor.
What is donor swapping ?
Donor swapping means the exchange of donors between two families that are not able to find a suitably matched donor within their family, but their mutual donors match the other family's recipients. In such situations donor from one family can donate the kidney to the recipient of the other family and vice versa.
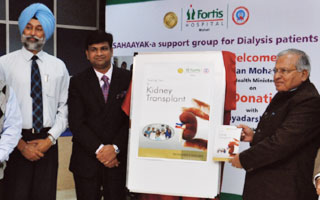
( Dr Priyadarshi Ranjan has pioneered the Kidney Transplant programme, at Fortis Hospital, Mohali. With vast experience of performing over 500 surgeries including kidney cancer, laparoscopic donor nephrectomies and kidney transplantation, his key areas of working include modern laparoscopic treatment for kidney diseases )











